Summary
– Acute bronchitis in babies and children
– Acute bronchitis in adults
– Exacerbations of chronic bronchitis
– Antibiotics prescribed
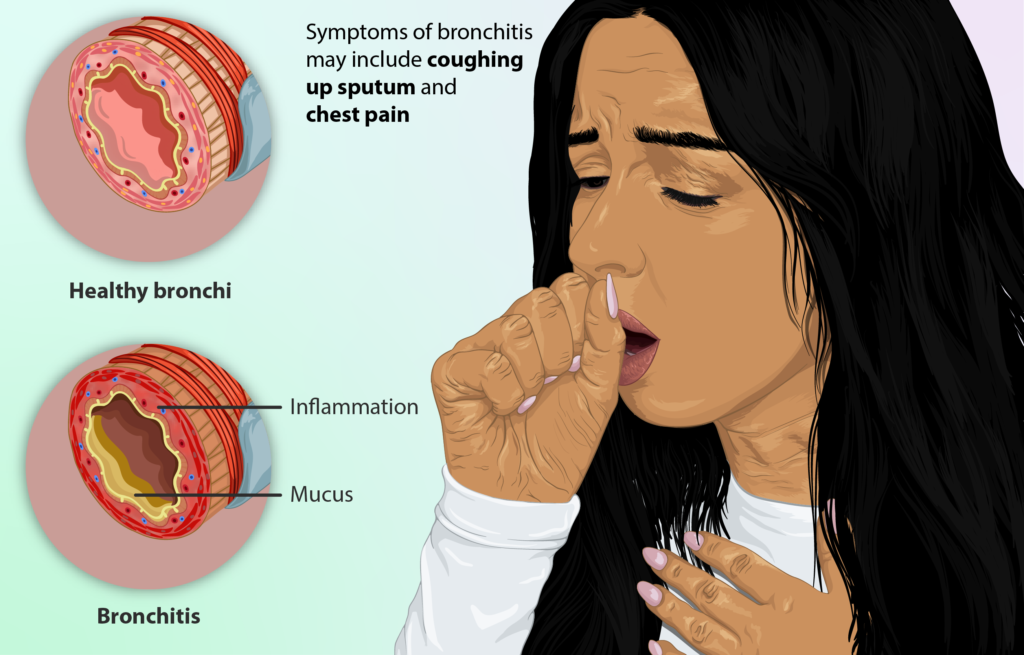
Acute bronchitis is an infectious pathology, most often of viral origin. The use of antibiotics (drugs to fight bacterial infections) is relatively rare and ineffective in bronchitis. Also, chronic bronchitis is not an infectious disease and therefore cannot be directly treated with antibiotics.
On the other hand, chronic bronchitis sufferers have more or less frequent episodes of acute bronchitis (exacerbations). Some of these exacerbations are of bacterial origin and require antibiotic treatment.
Acute bronchitis in babies and children
Acute bronchitis in babies and children is prevalent, as is bronchiolitis. These lower respiratory infections are most often viral in origin. Antibiotics are therefore ineffective in treating these diseases.
Acute bronchitis is benign in healthy babies and children and heals spontaneously in 2 to 3 weeks. However, special care must be taken in certain circumstances:
– In fragile children or those with serious illnesses (identified respiratory or cardiac disease): bronchitis can quickly become complicated by a bacterial superinfection requiring treatment with antibiotics.
– If a high fever persists (over 38.5°C) for at least 3 days, a doctor should be consulted to verify the diagnosis of bronchitis. In particular, pneumopathy should be ruled out, which may require antibiotic treatment.
In general, you should also be concerned if the baby:
– is an infant less than 6 weeks old;
– is premature and less than 3 months old;
– is drinking less than half of her bottles at three consecutive feedings;
– vomits systematically;
– sleeps all the time or, on the contrary, cries unusually and cannot fall asleep.
Acute bronchitis in adults
Acute bronchitis in healthy adults is a widespread lower respiratory infection. This disease is very often of viral origin, and antibiotics are therefore totally ineffective. Studies have clearly shown that antibiotics have no effect on the:
– evolution and duration of bronchitis;
– risk of bronchial superinfection;
– risk of complications.
The medical rule is, therefore, not to prescribe antibiotics in healthy adults. In adults with chronic severe diseases, the need for antibiotic therapy is discussed on a case-by-case basis, depending on the patient’s health status.
Acute bronchitis is usually mild and heals spontaneously in about ten days, although the cough may persist for a couple of weeks. Purulent sputum is not necessarily a sign of bacterial superinfection. However, in certain circumstances, it is essential to consult a doctor to evaluate the interest in antibiotic therapy:
– When the fever remains above 38.5°C for at least 3 days:
◦ The diagnosis of bronchitis should be confirmed, and the risk of pneumonitis should be ruled out.
◦ Bronchitis may be of bacterial origin: a few bacteria rarely cause acute bronchitis (Mycoplasma pneumonia, Chlamydia pneumonia, and Bordetella pertussis); treatment with antibiotics will then be necessary.
– If the cough persists for more than 3 weeks, additional tests are prescribed. In particular, pertussis should be ruled out in unvaccinated patients.
Exacerbations of chronic bronchitis

Exacerbations of chronic bronchitis are not always of infectious origin. When they are contagious, they may be viral (most often) or bacterial. The prescription of antibiotics is therefore limited and reserved for certain circumstances.
The use of antibiotics is based on
– the type of exacerbation of bronchitis;
– the likely bacterial origin of the exacerbation
– the patient’s lung function before the exacerbation.
Chronic bronchitis exacerbations are classified into 3 categories for antibiotic use:
– Simple chronic bronchitis exacerbation: antibiotics are not recommended, even in the presence of fever.
– Exacerbation of chronic obstructive bronchitis: antibiotics are reserved for patients with specific symptoms: worsening respiratory discomfort, frankly greenish secretions, an apparent increase in the volume of sputum, coexistence of another disease in the patient.
– Exacerbation of chronic obstructive bronchitis with chronic respiratory failure: antibiotics are systematically prescribed.
In all cases, a reassessment of the patient’s health status is necessary after 2 to 3 days of evolution of the exacerbation. Antibiotic therapy may become necessary during this reassessment if the fever remains above 38.5°C for at least 3 days.
However, it should be noted that these basic principles do not apply systematically. In the context of the COVID-19 epidemic, in particular, it is a virus, and therefore antibiotics are unnecessary. Also, exacerbating severe chronic bronchitis with worsening symptoms following SARS-CoV-2 infection can lead to a severe form of COVID-19.
These life-threatening patients are placed in an induced coma and placed on ventilator support for the duration of their treatment to allow them to receive oxygen. In this case, they may also receive antibiotics because of the risk of co-infection.
Antibiotics prescription
When acute bronchitis or an exacerbation of chronic bronchitis requires treatment with antibiotics, the choice of antibiotic depends on the patient’s health status:
– the status of lung function;
– the frequency of exacerbations (less than or more than 3 per year);
– the existence of another pathology in the patient.
The antibiotics chosen must be active on the bacteria most often involved in bacterial superinfections: Streptococcus pneumoniae (pneumococcus), Hæmophilus influenzæ, Branhamella catarrhalis.
Generally, doctors choose the antibiotic from the following two groups:
– Group 1 includes antibiotics that can be used as first-line antibiotics when exacerbations are few (no more than 3 per year) or for acute bronchitis requiring antibiotic therapy:
◦ amoxicillin (penicillin, this is the standard antibiotic used in the first line);
◦ cephalosporins (cefalexin, cefadroxil, cefaclor, cefatrizine) as a second choice ;
◦ macrolides (erythromycin, spiramycin, josamycin, roxithromycin, clarithromycin, dirithromycin, azithromycin), pristinamycins, or doxycycline, as alternatives in case of allergy to penicillins.
– Group 2 includes antibiotics that can be used in case of failure of first antibiotic treatment, when exacerbations are frequent (more than 4 per year), or if the patient’s respiratory function is significantly reduced:
◦ amoxicillin combined with clavulanic acid (reference antibiotic);
◦ cephalosporins (cefuroxime, cefpodoxime, cefotiam) in oral form;
◦ certain fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin, which are the antibiotics most strongly associated with an increase in resistance, bearing in mind that moxifloxacin, which is no more effective than others, exposes to Lyell’s syndromes, fulminant hepatitis, and an increase in cardiac disorders).
Note: all of these antibiotics are administered orally, with a dosage adapted to the age. The duration of antibiotic therapy varies from 7 to 10 days, with a shorter period of 5 days for certain antibiotics.
For example, azithromycin is cardiotoxic and should never be used in combination with hydroxychloroquine to combat the bronchial symptoms caused by COVID-19, leading to rhythm or cardiac conduction disorders and sometimes fatal cardiac arrests.